Hepatic Coma or Hepatic Encephalopathy (HE)
Hepatic Coma or Hepatic Encephalopathy (HE)
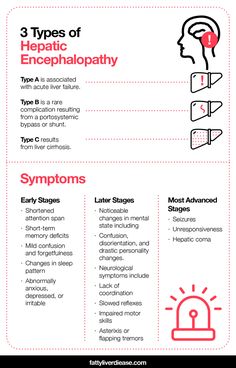
Definition: Hepatic encephalopathy is a neuropsychiatric syndrome caused by liver dysfunction, leading to the accumulation of toxins (especially ammonia) in the blood, which can impair brain function. In severe cases, it can progress to hepatic coma.
Causes: HE typically occurs in individuals with advanced liver disease, especially cirrhosis or acute liver failure. Triggers that exacerbate the condition include:
- Gastrointestinal bleeding
- Infection
- Electrolyte imbalance (especially low potassium)
- High protein intake
- Constipation
- Dehydration
- Certain medications (e.g., sedatives or diuretics)
Pathophysiology:
- The liver usually detoxifies ammonia (NH₃) by converting it into urea, which is excreted in urine.
- In liver failure, ammonia builds up in the bloodstream and crosses the blood-brain barrier, leading to neurological impairment.
- Other toxins, inflammatory mediators, and metabolic disturbances contribute to the development of encephalopathy.
Stages of Hepatic Encephalopathy:
- Stage I (Mild): Subtle cognitive and behavioral changes, such as forgetfulness, mild confusion, irritability, and impaired attention.
- Stage II (Moderate): More severe confusion, disorientation, lethargy, and personality changes (e.g., inappropriate behavior).
- Stage III (Severe): Marked confusion, somnolence, inability to follow commands, and slurred speech.
- Stage IV (Coma): The patient becomes unresponsive and enters a coma. This is a medical emergency, requiring immediate intervention.
Symptoms:
- Cognitive dysfunction: confusion, forgetfulness, difficulty concentrating
- Asterixis: flapping tremor of the hands
- Altered sleep-wake patterns: insomnia or hypersomnia
- Slurred speech, slow movement
- Behavioral changes: agitation, irritability, euphoria, or lethargy
- In severe cases: coma and death
Diagnosis:
Clinical Examination:
- Mental status assessment using tools like the West Haven Criteria.
- Observation for asterixis (flapping tremor).
Laboratory Tests:
- Elevated serum ammonia levels (although not directly correlated with HE severity).
- Liver function tests (e.g., ALT, AST, bilirubin).
- Electrolyte and blood gas analysis.
Neuroimaging:
- CT or MRI to rule out other causes of neurological impairment, such as stroke or head injury.
Management:
Correction of Precipitating Factors:
- Treating infections, electrolyte imbalances, and gastrointestinal bleeding.
- Adjusting medication regimens (e.g., stopping sedatives).
Reducing Ammonia Levels:
- Lactulose: A non-absorbable sugar that traps ammonia in the gut and promotes its excretion.
- Rifaximin: An antibiotic that decreases ammonia-producing gut bacteria.
- Low protein diet: To reduce ammonia production from protein metabolism.
Supportive Care:
- Monitoring mental status and liver function.
- Ensuring adequate hydration and nutritional support.
- Managing complications like cerebral edema in advanced cases.
Liver Transplantation:
- The only definitive treatment for HE caused by irreversible liver failure.
Prognosis:
- The prognosis depends on the underlying liver disease and how promptly precipitating factors are addressed.
- Without treatment, HE can progress to coma and death. Long-term outcomes improve significantly with liver transplantation in end-stage liver disease patients.
Prevention:
- Early detection and management of liver disease.
- Avoidance of known precipitants like alcohol and hepatotoxic drugs.
- Regular monitoring for ammonia levels and neurological function in patients with chronic liver disease.
Nursing Management of Hepatic Encephalopathy
1. Monitoring and Assessment:
- Neurological status: Regularly assess the patient's level of consciousness, orientation, and cognitive function. Utilize scales like the Glasgow Coma Scale (GCS) or West Haven Criteria to quantify changes in mental status.
- Vital signs: Frequent monitoring of vital signs, especially blood pressure, heart rate, and respiratory status, since hypotension or respiratory distress may occur in advanced HE.
- Signs of asterixis: Check for flapping tremors, which are often present in the earlier stages of HE.
- Lab monitoring: Regularly assess serum ammonia levels, liver function tests (LFTs), electrolytes, and coagulation profiles to detect worsening hepatic function or metabolic derangements.
- Intake and output: Ensure accurate recording of fluid intake and output to detect dehydration or fluid overload, which can worsen encephalopathy.
2. Nutritional Management:
- Protein intake adjustment: Patients with HE may require a controlled or reduced protein diet to minimize ammonia production. However, severe protein restriction should be avoided to prevent malnutrition.
- Enteral nutrition: If the patient is unable to eat, consider administering enteral feeds with a carefully balanced protein composition.
- Hydration: Ensure the patient remains well-hydrated, especially if they are on diuretics or lactulose, which can cause dehydration and electrolyte imbalances.
3. Medication Administration:
- Lactulose: Administer lactulose as prescribed to reduce ammonia levels. The goal is to induce 2-3 soft bowel movements daily to prevent constipation, which can exacerbate HE.
- Monitor for signs of diarrhea, dehydration, and electrolyte imbalances, adjusting doses as necessary.
- Rifaximin: Ensure compliance with antibiotics like rifaximin, used to reduce the bacterial production of ammonia in the gut.
- Electrolyte correction: Monitor and correct electrolyte disturbances, particularly hypokalemia and metabolic alkalosis, which can exacerbate encephalopathy.
4. Infection Control:
- Patients with HE are prone to infections due to weakened immune function.
- Monitor for infection: Regularly check for signs of infections such as fever, chills, and elevated white blood cell counts.
- Sterile techniques: Use strict aseptic techniques when performing invasive procedures like intravenous line insertions or urinary catheterizations.
5. Preventing Complications:
- Fall precautions: Patients with altered mental status are at high risk for falls. Implement fall prevention strategies, such as using bed alarms and keeping the bed in a low position.
- Airway protection: As the patient's mental status declines, their ability to protect their airway may be impaired, increasing the risk of aspiration. Monitor for signs of aspiration pneumonia and, if necessary, prepare for intubation in severe cases.
- Seizure precautions: Patients with severe encephalopathy may develop seizures. Keep seizure pads on the bed and ensure emergency medication like benzodiazepines is available.
6. Family and Patient Education:
- Explain HE progression: Educate the patient and family about the symptoms of hepatic encephalopathy and its triggers, helping them understand how to prevent worsening episodes.
- Dietary management: Provide dietary counseling to encourage adherence to the recommended low-protein diet.
- Medication adherence: Stress the importance of taking medications like lactulose regularly to prevent the recurrence of HE.
- Alcohol abstinence: Emphasize avoiding alcohol or hepatotoxic substances if the underlying cause is related to liver cirrhosis or alcohol abuse.
7. Psychosocial Support:
- Coping strategies: Provide emotional support to both the patient and their family as hepatic encephalopathy can be distressing.
- Support groups: Encourage participation in liver disease support groups for long-term management and coping with chronic illness.
8. Coordination of Care:
- Multidisciplinary collaboration: Work closely with the medical team, dietitians, pharmacists, and physiotherapists to ensure comprehensive care for the patient.
- Plan for discharge: Once the patient is stabilized, collaborate on discharge planning, ensuring they have adequate support at home and know when to seek medical help.
Case Study Example:
Case: A 55-year-old male with a history of alcoholic cirrhosis is admitted with confusion, drowsiness, and a flapping tremor in both hands (asterixis). He had been non-compliant with his lactulose regimen for several days and experienced recent constipation. His family reports a recent increase in protein consumption. Lab results show elevated ammonia levels, mild hypokalemia, and a decrease in albumin levels.
Nursing Actions:
- Administer lactulose and ensure bowel movements are occurring to decrease ammonia levels.
- Monitor the patient's neurological status every 4 hours using the GCS and asterixis assessments.
- Administer IV potassium supplements to correct the hypokalemia.
- Educate the family on the importance of medication adherence and dietary restrictions.
- Prevent potential complications by implementing fall precautions, and monitoring for aspiration, as the patient is somnolent.
- Collaborate with the physician to adjust medications and create a comprehensive discharge plan.










Comments
Post a Comment