MALNUTRITION
MALNUTRITION
Malnutrition
Malnutrition includes both under nutrition - acute
malnutrition (i.e. wasting and/or nutritional oedema), chronic malnutrition
(i.e. stunting), micronutrient malnutrition and inter-uterine growth
restriction (i.e. poor nutrition in the womb) -and over nutrition (overweight
and obesity.
Acute malnutrition or wasting (and / or oedema) occurs when
an individual suffers from current, severe nutritional restrictions, a recent
bout of illness, inappropriate childcare practices or, more often, a
combination of these factors. It is characterized by extreme weight loss,
resulting in low weight for height, and/or bilateral oedema,
and, in its severe form, can lead to death. Acute malnutrition
reduces resistance to disease and impairs a whole range of bodily functions.
Acute malnutrition may affect infants, children and adults. It is more commonly
a problem in children under-five and pregnant women,
but nonetheless this varies and must be properly assessed in each context.
Levels of acute malnutrition tend to be highest in children from 12 to 36
months of age when changes occur in the child’s life such as rapid weaning due
to the expected birth of a younger sibling or a shift from active breastfeeding
to eating from a family plate, which may increase vulnerability.
The most visible consequences of acute malnutrition are weight loss
(resulting in moderate or severe wasting) and/ or nutritional oedema (i.e.
bilateral swelling of the lower limbs, upper limbs and, in more advanced cases,
the face). Acute malnutrition is divided
into two main categories of public health significance: severe acute malnutrition (SAM) and moderate acute malnutrition (MAM). MAM is characterised by moderate
wasting. SAM is characterised by severe wasting and/or nutritional oedema.
The term global acute malnutrition
(GAM) includes both SAM and MAM. Mild acute malnutrition also has consequences
but is not widely used for assessment or programming purposes.
Acute
malnutrition increases an individual’s risk of dying because it compromises
immunity and impairs a whole range of bodily functions. When food intake or utilisation (e.g.
due to illness) is reduced, the body adapts by breaking down fat and muscle
reserves to maintain essential functions, leading to wasting. The body also
adapts by decreasing the activity of organs, cells and tissues, which increases
vulnerability to disease and mortality. For reasons not completely understood,
in some cases, these changes manifest as nutritional oedema.
A ‘vicious cycle’ of disease and malnutrition is often observed once these adaptations
commence.
Moderate Acute Malnutrition (MAM)
The burden of MAM (wasting) globally is
considerable. Around 41 million children are moderately wasted worldwide and
the management of MAM is finally becoming a public health priority, given this
increase in mortality and the context of accelerated action towards achievement
of Millennium Development Goals (MDGs) 3 and 4. Children with MAM have a
greater risk of dying because of their increased vulnerability to infections as
well as the risk of developing SAM, which is immediately life threatening.
Some children with MAM will recover spontaneously
without any specific external intervention; however the proportion that will
spontaneously recover and underlying reasons are not well documented.
8.2
Severe Acute Malnutrition (SAM)
Acute
malnutrition is distinguished by its clinical characteristics of wasting and /
or bilateral pitting oedema
- Marasmus – severe wasting presenting as
both moderate and severe acute malnutrition
- Kwashiorkor
–
bloated appearance due to water accumulation (nutritional bilateral
pitting oedema)
- Marasmic kwashiorkor- is a condition which combines
both manifestations.
It
usually develops rapidly as a result of protein deficiency, or more commonly,
it is precipitated by an illness such as measles or other infections. It occurs
mainly in older infants and young children aged 1 to 3 years.
Clinical signs
- Poor growth characterized by loss
of weight and growth failure (60 to 80% weight for age).
- Oedema- accumulation of fluids in
tissues causing swelling
- Wasting of muscles
- Mental changes characterized by
apathy, misery, irritability and sadness.
- Hair changes- the hair becomes
coarse, lack of luster, brownish, sparse and easily pulled out.
- Anaemia due to lack of protein to
synthesize blood cells is worsened by iron deficiency, malaria and worm
infestation.
- Skin changes/lesions- dark
pigmentation in areas of friction i.e. patches like sun burns.
- Diarrhoea
- Moon face-cheeks appear swollen
with fatty tissues or fluids.
- Poor appetite/ anorexia
- Hepatomegaly (enlarged fatty
liver).
8.2.2 Marasmus (Chronic PEM)
Occurs commonly in children from 6 to 18 months of age. The
deficiency is primarily due to lack of energy especially in starvation and is
worsened by infections and parasitic diseases.
Clinical signs
- Growth failure (weight for age
less than 60%)
- Severe muscle wasting
- Alert though with deep sunken eyes
- Good appetite (violent suckling of
hands)
- The face is wrinkled and drawn in
( look like an old man)
- Diarrhoea
- Dehydration.
It
is a mixed form of PEM, and manifests as oedema occurring in children who may
or may not have other signs of kwashiorkor. It reflects as a deficiency of both
energy and protein.
8.2.3.1 Clinical signs
- Flaky paint dermatitis
- Mental changes
- Hepatomegaly
- Diarrhoea
- Dehydration
- Oedema
Prevention of PEM
PEM can be prevented by:
a.
Giving
children adequate food that is energy and micronutrient dense.
b.
Exclusively
breastfeeding infants for the first six months and then introduction of
nutritious complementary foods starting at six months with continued
breastfeeding up to two years and beyond.
c.
Preventing
or treating infectious diseases promptly since they increase nutrient needs.
d.
Deworming
children to eradicate worm infestations which contribute to low nutrient
utilization.
e.
Enhancing
proper sanitation when handling, preparing and feeding children to prevent
contamination. The water used to prepare feeds should be clean.
f.
Promoting
good maternal nutrition since it contributes to the health outcome of the baby.
Poor maternal nutritional status leads to delivering preterm and low birth
weight babies who are at risk of developing PEM.
g.
Promoting
health education especially among the care givers of children.
Micronutrient Deficiencies
Micronutrients are minerals and vitamins that are needed in
tiny quantities (and are therefore known as micronutrients). Micronutrient deficiencies account for roughly 11%
of the under-five death burden each year.It is now recognised that poor growth
in under-fives results not only from a deficiency of protein and energy but
also from an inadequate intake of vital minerals (e.g., zinc), vitamins, and
essential fatty acids.
Vitamins are either water-soluble
(e.g. the B vitamins and vitamin C) or fat-soluble (e.g. vitamins A, D, E and
K). Essential minerals include iron, iodine, calcium, zinc, and selenium
Key
micronutrient deficiencies
· Iron deficiency leads to iron
deficiency anaemia
· Vitamin C deficiency leads to scurvy
·
Vitamin
A deficiency leads to xerophthalmia
·
NiacinorVitamin B3 deficiency leads
topellagra
· Iodine deficiency leads to goitre and
cretinism (in infants born to iodine deficient mothers)
· Thiamin or B1 deficiency leads to
beriberi
· Riboflavin
deficiency leads to ariboflavinosis
· Vitamin D deficiency leads to rickets
The main cause of micronutrient
malnutrition is usually an inadequate dietary intake of vitamins and/or
minerals.
Causes of Malnutrition
UNICEF’S conceptual framework on the causes of malnutrition:
a.
Immediate causes: Inadequate food intake and presence
of disease
b.
Underlying causes: inadequate household food security;
inadequate maternal and child care; inadequate health services and unhealthy
environment
c.
Basic causes: resources and control; human;
economic and organizational; political and ideological superstructure;
potential resources; technology;
environment; people
Conceptual Framework of
Malnutrition
The basic causes of malnutrition are greatly influenced by:
- Political situations and economic
systems that determine how resources are distributed
- Legal factors that determine how
far the rights of women and girls are protected by law
- Cultural factors i.e. the ideologies and policies governing
social sectors
To address basic causes of malnutrition, greater and better
targeted resources and better collaboration are needed between sections of
national governments and donors. United Nations Agencies, non-governmental
organizations and investors. Above all, the poor themselves must be a major
part of the process.
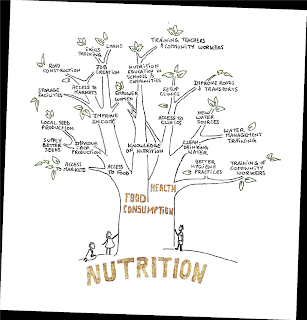
Solution Tree
To address the problem of malnutrition, a multi-sectoral approach is used. Many sectors work together to address the different causes.
The
preparation of a solution tree will present “Reduction of malnutrition” as a
common objective for an integrated approach addressing the various causes of
malnutrition, bringing together different technical departments within an
organization, or highlighting potential partnerships between organizations with
complementary expertise. A health agency providing nutrition treatment, for
example, could partner with a food security agency that will assist patients’
families in diversifying their food production, income sources and food
consumption, thus preventing relapses. Not only does the use of nutrition as a
common objective facilitate the identification of cross-sectoral linkages, it
also carries meaning.


.jpg)
Comments
Post a Comment